
Practical guidance on Vape implications and mapping to electronic cigarette icd 10 concepts
This comprehensive resource explores the clinical, coding and documentation strategies for clinicians, coders, auditors and health information professionals who encounter patient encounters related to vaping. The word Vape appears intentionally throughout the text to optimize search relevance for readers looking for specialized guidance on electronic cigarette icd 10 classification, while the material remains clinically focused, evidence-informed and practical for everyday health record workflows.
Understanding the clinical spectrum of vaping-related presentations is the first step in accurate classification. A patient who uses an e-cigarette may present with a variety of issues: nicotine dependence or withdrawal, acute or chronic respiratory symptoms, dermatologic reactions, cardiovascular complaints, gastrointestinal upset or accidental ingestion/poisoning. Coding professionals should identify the primary reason for the encounter, whether it is an acute injury, a chronic disease exacerbation, preventive counseling, or a poisoning event, because the main clinical descriptor determines sequencing and code selection in most coding conventions.
Core principles for mapping vaping encounters to ICD-10
- Document the clinical focus: If the visit is for nicotine dependence, capture the dependence diagnosis and any related behavioral counseling or pharmacotherapy. If the visit is for an acute lung injury, prioritize the respiratory diagnosis and capture the exposure to aerosols/e-cigarette products as an important contributing element.
- Use symptom and manifestation codes when necessary: When a definitive diagnosis is pending, document and code the presenting symptoms (e.g. cough, wheeze, chest pain, shortness of breath) and link them to vaping exposure in the medical record to support later code refinement.
- Sequence by coding guidelines: Apply standard sequencing rules – primary diagnosis is the condition chiefly responsible for the encounter. Secondary codes can document nicotine use, dependence, poisoning, or external causes related to product use.
- Avoid assumptions: Do not assume causality without clinical evidence. Record the clinician’s assessment, suspected links, and any diagnostic testing that supports a vaping-related etiology.


Which ICD-10 categories are most relevant?
When considering electronic cigarette icd 10 options, several diagnostic families commonly apply. Use this as an organizational map rather than a checklist of exact code numbers: F-codes for substance-related conditions (for example, nicotine dependence documented as a tobacco/nicotine-related behavioral health diagnosis), J-codes for respiratory conditions (acute bronchitis, chemical pneumonitis, or other inhalation-related lung injury), and T-codes for poisonings or toxic effects when ingestion or acute toxicity is evident. Additionally, include external cause codes or supplemental documentation indicating product exposure, device injury, or self-directed harm when appropriate to the clinical scenario.
Clinical examples to guide coding logic
- Outpatient counseling for e-cigarette cessation: Primary diagnosis could be nicotine dependence (document the type of tobacco product used), with an additional code to reflect counseling or behavioral therapy if billable.
- Emergency visit for acute respiratory distress with a history of recent vaping: Primary code should reflect the acute respiratory condition (e.g., chemical pneumonitis, hypoxia) with a secondary notation of recent e-cigarette exposure in the clinical history to support linkage and any potential public health reporting.
- Pediatric ingestion of e-liquid: Code the toxic effect or poisoning as primary, document route (ingestion), product (nicotine e-liquid), and provide details on circumstances and treatment provided; these details guide correct T-code selection and emergency care reimbursement.
Documentation essentials for accurate coding
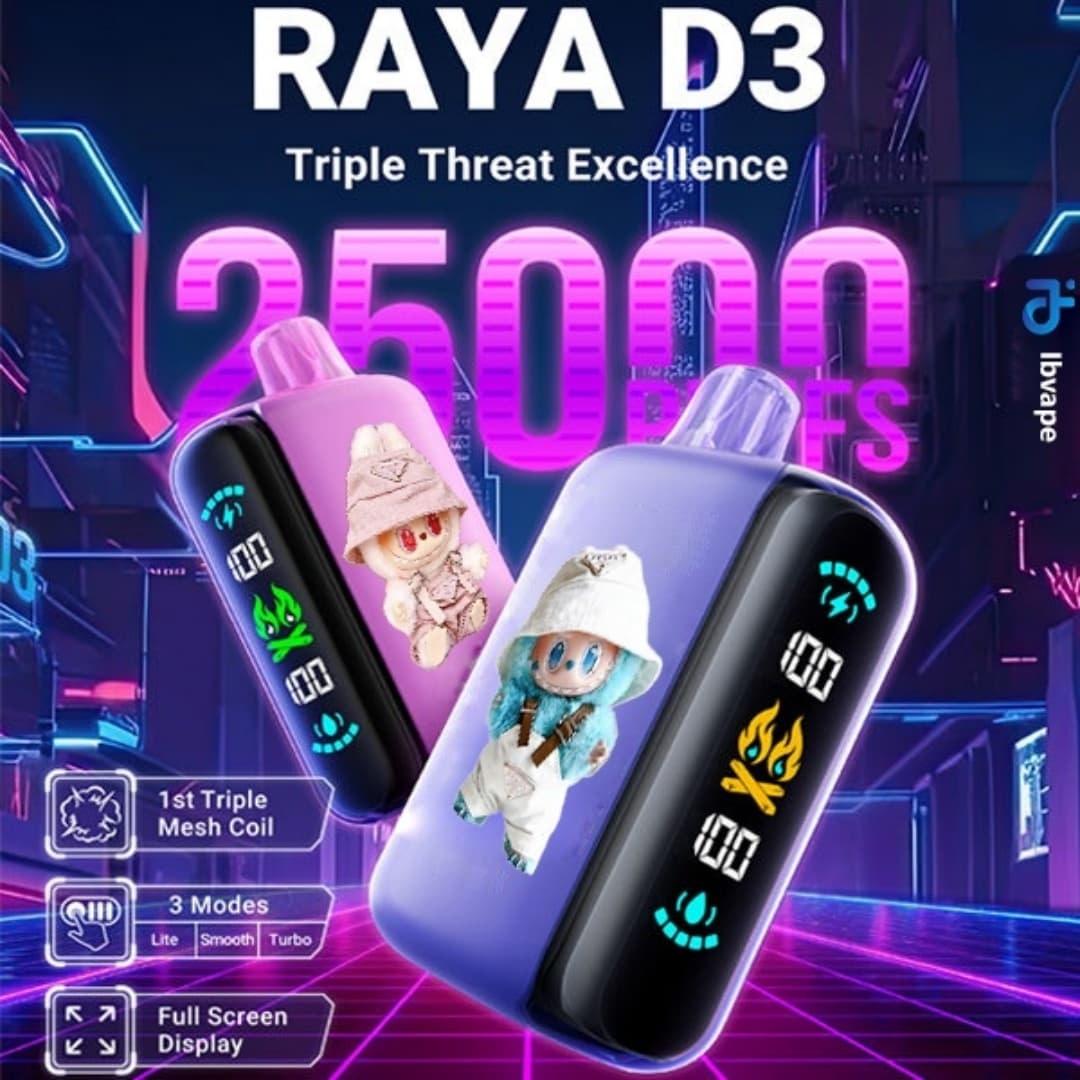
High-quality documentation is the cornerstone of precise electronic cigarette icd 10 mapping. Clinicians should be guided to record the following: type of product used (disposable vs refillable device, nicotine concentration or strength when known), frequency and duration of use, recent changes in product or protocols (new flavors or additives, home modifications), symptom timeline relative to product exposure, objective findings (vital signs, oxygen saturation, imaging results), interventions (oxygen therapy, bronchodilators, corticosteroids, antidotes), and disposition. Explicit language such as “due to,” “suspected secondary to,” or “likely related to” helps coders decide whether to use a causal link or simply document concurrent conditions. When causation is uncertain, many coding systems recommend documenting the presenting condition as primary and listing suspected contributing exposure as secondary or as history/observation evidence.
Tip: Encourage clinicians to use structured templates or checklists that prompt for product specifics and exposure timing — that small addition dramatically improves coding accuracy and public health surveillance.
Billing, reimbursement and payer considerations
From a reimbursement perspective, payers evaluate both the medical necessity of treatment and the precision of diagnostic codes. Claims that specify a clear clinical problem (e.g., acute chemical pneumonitis) with supportive documentation are more likely to be adjudicated favorably than claims using nonspecific symptom codes without exposure context. For preventive services, counseling and tobacco cessation programs associated with e-cigarette cessation may be reimbursable when documented properly — include time spent, counseling modality (individual, group, telephone), and any pharmacologic prescriptions for nicotine replacement therapy or approved cessation medications.
Public health reporting and surveillance
Many health systems and public health agencies track vaping-associated illnesses or clusters of lung injury. Accurate capture of Vape exposures in the electronic health record facilitates case finding and trend analysis. Coders should help ensure the exposure is captured in the record even when a definitive diagnosis is pending. Timely communication between clinical teams and coding/audit staff is essential when novel patterns of illness emerge that may require special reporting or specific coding conventions adopted by public health authorities.
Practical coding tips for specialists and auditors
- Crosswalk symptoms to likely organ system codes first, then use secondary codes to document exposure to Vape products.
- When a clinician documents “nicotine dependence” or “e-cigarette dependence,” ensure the record includes product type and frequency to support the substance-related diagnosis.
- When the encounter is preventive counseling, code for cessation counseling plus any applicable preventive counseling codes rather than coding only for routine office visits.
- For poisoning or toxic effects, include route (ingestion, inhalation, dermal exposure), intent (accidental, intentional), and encounter type (initial, subsequent, sequela) as these modifiers directly influence code selection and sequence.
- Use problem lists and social history fields in EHRs to consistently capture ongoing e-cigarette use — this facilitates case-mix reporting and chronic disease registries.
Education and coder-clinician collaboration
Health information teams should provide targeted education to clinicians about documentation points that materially affect electronic cigarette icd 10 assignment. Regular feedback loops, coding clinics, and simple one-page documentation tips improve coder confidence and reduce denials. Coding teams must also stay current with official coding guidance and any advisories from authoritative organizations that might introduce new codes or clarifications specific to vaping-related illnesses.
Quality assurance and audit strategies
Audit plans should sample charts with vaping exposure and assess concordance between documentation and coded data. Key audit checks include validation of causality statements, presence of objective testing when used to justify certain diagnoses, appropriate sequencing, and whether external cause or product exposure details are captured when required. Tracking trends across episodes — such as an uptick in respiratory diagnoses tied to vaping exposure — can inform targeted education and public health action.
Patient communication and preventive messaging
Clinical encounters are opportunities to educate patients about risks associated with Vape devices, nicotine toxicity, the dangers of unregulated additives and the importance of safe storage to prevent accidental ingestion. Documenting counseling, educational materials provided, and follow-up planning not only supports patient care but also clarifies the medical necessity of services rendered for coding purposes.
Emerging issues and future directions
As products and use patterns evolve, so will clinical presentations and coding needs. Health systems should monitor coding guidance updates and participate in data-sharing initiatives that track long-term trends in vaping-related morbidity. Investment in EHR templates that capture product-level detail (device, brand, nicotine concentration) will improve coding granularity and support better research and surveillance.
Key takeaways:
- Identify the primary clinical problem first, then use secondary codes to document nicotine use, exposure to Vape products or toxic effects.
- Use symptom and organ-system codes when diagnoses are not yet established but ensure exposure details are recorded.
- Support clinicians with documentation tools and coder education to improve the quality and accuracy of electronic cigarette icd 10 capture across care settings.
References and resources for ongoing learning
Consult official coding guidelines, payer policies, and clinical advisories from professional organizations for the most current coding rules and recommended practices. Regular participation in coding forums and coding clinics focused on substance-related and inhalation injury coding can also be valuable.
FAQ
If the visit is unrelated to vaping, document the e-cigarette use in the social history or problem list and code it as a secondary or history code when relevant to care. Do not sequence it as primary if it is not the reason for the encounter.
Q2: What documentation supports coding a vaping-related lung injury?
Document onset of symptoms relative to vaping exposure, objective findings (imaging, oxygenation), clinician assessment linking exposure to the condition, and any treatments given; this narrative supports selection of a respiratory diagnosis with an exposure-related secondary code.
Q3: Are there special codes for e-liquid ingestion in children?
Yes, poisoning and toxic effect codes should be used with details about route, intent and encounter type; ensure emergency care details and product information are recorded to justify the chosen toxicology code.
